A conference to discuss advanced techniques to fight cancer.
Résumé
ICTR-PHE : unir la physique, la médecine et la biologie
La conférence ICTR-PHE 2014 a réuni à Genève quelque 400 participants du monde entier venus discuter des dernières techniques de lutte contre le cancer. Chercheurs et praticiens de nombreuses disciplines ont passé en revue les dernières avancées de la recherche translationnelle, grâce à laquelle les innovations de la recherche fondamentale trouvent des applications dans le domaine de la santé (physique, biologie ou oncologie clinique). Pour tous les spécialistes concernés, la conférence ICTR-PHE est l’endroit idéal pour faire le point des travaux réalisés jusque-là et définir les prochaines étapes afin de maintenir la dynamique.

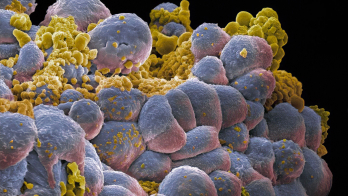
Image credit: Nymus3d/ENVISION.
Physicists, biologists, physicians, chemists, nuclear-medicine experts, radio-oncologists, engineers and software developers – researchers and practitioners from many disciplines came to Geneva on 10–14 February for ICTR-PHE 2014, which brought together for the second time the International Conference on Translational Research in Radio-Oncology and Physics for Health in Europe. The joint conference aims to unite physics, biology and medicine for better healthcare, and the goal of this second meeting was to review the most recent advances in translational research – where developments in basic research are “translated” into means for improving health – in physics, biology and clinical oncology.
The conference featured the many advances that have occurred during the past two years since the first joint conference. The resolution and precision of medical imaging is continuing to grow with the use of combined modalities, such as positron-emission tomography (PET) with computed tomography (CT), and PET with magnetic resonance imaging (MRI) – an important technical breakthrough. Biologists and chemists are performing studies to develop new radiation carriers – including antibodies and nanoparticles – to target tumours. The Centro Nazionale di Adroterapia Oncologica (CNAO) in Italy has started hadron therapy with proton beams and carbon-ion beams, obtaining the necessary certification labels for both treatments. Another new centre, MedAustron in Austria, is being built and is reaching the commissioning phase. Moreover, while the use of proton therapy continues to grow around the world, the Japanese centres and the Heidelberg Ion-Beam Therapy Centre in Germany are using carbon-ion therapy on an increasing number of patients. For all of the experts involved in such a variety of different fields, the ICTR-PHE conference was the ideal place to take stock of the work done so far, and to define the next steps that the community should take to keep the momentum high.
Although the first patient was treated with protons 60 years ago in Berkeley, the field has not yet implemented all of the phases of the clinical trials required for evidence-based medicine and the national health systems. In particular, several experts discussed the need to perform randomized trials. This, of course, comes with unavoidable ethical issues and methodological concerns. The community is geographically scattered and several important factors – such as the integrated dose that should be delivered, the fractionation and the types of tumours to be treated – are still being studied. On one hand, it is a hard task for the various scientists to define common protocols to be followed to perform the trials. On the other hand, physicians and patients might be sceptical towards new therapies that are not yet felt to be tested extensively. Despite the fact that every year several thousand patients are diagnosed using radiopharmaceuticals and subsequently treated with hadron therapy, the use of particles is still often considered with scepticism.
The situation is made even more complex by the fact that the fight against cancer is taking on a more personalized approach. Although highly beneficial to patients, this makes it difficult for doctors to apply the same treatment plan to a large number of people. Cancer is not really a single disease. Its many facets require different therapies for different patients, depending on the specific type of malignant cell, the location of the tumour, its dimensions, etc. Several presentations at the conference focused on the important impact that such personalized treatment has in the disease’s prognosis.
In this respect, the challenge for today’s oncologists starts with high-quality imaging that allows them to define the active tumour volume as well as the possible metastasis in the body. Again, depending on the type of tumour, researchers can now select the best radiopharmaceutical that, once injected into the body and in conjunction with a detection modality such as PET, is able to identify the target cells precisely. Moreover, the same carrier molecules that are able to bring the radiating isotopes to the malignant cells and make them visible to the detecting instruments could be used with more powerful isotopes, to bring a lethal dose into the tumour volume directly. Some of the most recent studies involve the use of specific peptides associated with isotopes obtained at particle accelerators. Others involve innovative nanoparticles as vehicles to bring radiation into the target. Each single solution implies the use of specific isotopes. At CERN, the MEDICIS project aims to produce isotopes for medical research. Although the project has only recently entered the construction phase, the collaboration between the MEDICIS team and specialized teams of radiobiologists and chemists has already begun.

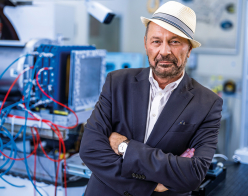
Image credit: CERN-PHOTO-201402-028 – 48.
Imaging has reached spatial resolutions down to 2 mm. The combination of various imaging techniques, such as PET/CT or PET/MRI, allows oncologists to gather information not only about the geometry of a tumour but also about its functionality. Further improvements could come from both better hardware and more sophisticated software and algorithms for integration of the information. Significant improvement to the hardware could be introduced by the time-of-flight technique – well known to particle physicists for its use in many high-energy experiments.
The best treatment
Once the oncologists have acquired the information about the malignant cells and tumour volume, as well as other important data about the patient, they can define the best treatment for a specific case. Computer simulations made with the GEANT4 and FLUKA software suites are used to define the most suitable treatment planning. These codes are in continuous development and are able to deliver increasingly precise information about the dose distribution. In addition to new advances in computer simulations, the ICTR-PHE conference also featured a presentation about the first 3D mapping over a known distance of the dose distribution along the whole path of a 62 MeV proton beam. These studies are extremely useful in the determination of collateral damage, including possible secondary tumours caused by particle beams.
Unwanted damage to healthy tissues is a key point when it comes to comparing conventional photon-radiation therapy with hadron therapy. Thanks to the intensity modulation and volumetric arc techniques, and image-guided treatments, today’s conventional radiation therapy has reached levels of effectiveness that challenge hadron therapy. Nevertheless, because of the specific way they deliver their energy (the well known Bragg peak), hadrons can target tumours much more precisely. Therefore, hadron beams are potentially much less dangerous to nearby healthy tissues. However, their overall biological impact is still to be evaluated precisely and the cost of the infrastructures is significantly higher than for widely used conventional radiation. The debate remains open, and a final word will only come once the various teams involved have carried out the necessary clinical trials. The importance of sharing information and data among all active partners was highlighted throughout the conference.
In general, the results presented at the conference were, in many cases, very promising. Not only has the knowledge of cancer increased hugely during recent years, in particular at the molecular level, but also – and even more importantly – a different awareness is gaining momentum within the various communities. As one of the plenary speakers emphasized, the idea that one single oncologist can effectively fight cancer should be abandoned. Instead, the collaboration among chemists, biologists, engineers, physicists and physicians should surely improve the prognosis and the end result.
The beneficial impact of such collaboration was particularly evident when the speakers presented results from the combination of various techniques, including surgery and chemotherapy. This is because several factors play a role in the response of malignant cells to radiation: drugs, of course, and also the patient’s immunology, the hypoxia (oxygen deprivation) rate and the inner nature of the tumour cells. Recent studies have shown, for example, that malignant cells infected by the HPV virus have a better response to radiation, which translates into a better prognosis.
The role played by hypoxia and the various ways to overcome it were popular topics. A particularly interesting talk emphasized the need to go a step further and, having already acquired a deep knowledge of hypoxia in the malignant tissues, proceed to treat it with drugs before starting any further therapies. This is not yet the case in the current protocols, despite the many confirmations coming from research studies.
Indeed, the time needed for a new medical advance developed by scientists to reach the patient is a key issue. In this respect, the ICTR-PHE conference has a unique role. Medical doctors can learn about the latest radio-pharmaceuticals, the latest imaging instruments and the latest therapies that other scientists have worked on. At the same time, physicists, specialized industry, radiobiologists, etc, can hear from the medical field where they should concentrate their efforts for future research.
The impression was that the community is very willing to build a new collaboration model and that CERN could play an important role. The newly created CERN Office for Medical Applications is an example of the strength of the laboratory’s wish to contribute to the growth of the field. Medical doctors need cost-effective instruments that are easy to use and reliable over time. This presents a challenge for physicists, who will have to use the most advanced technologies to design new accelerator facilities to produce the hadron beams for patient treatment.
In addition to new accelerators, there is a plethora of opportunities for the physics field. These include the construction of a biomedical facility at CERN to provide particle beams of different types and energies for external users for radiobiology and detector development; the construction and testing of innovative detectors for beam control and medical imaging; the development of state-of-the-art instruments for accurate dosimetry; the MEDICIS facility for the production of rare radioisotopes; and a powerful computing grid for image treatment and storage.
As one of the speakers said, quoting the novelist William Gibson: “The future is here. It is just not evenly distributed yet.” This is the next challenge for the community of scientists who attended ICTR-PHE 2014 – to take all of these advances to the patients as quickly as possible.
| Physics highlights |
|
Even though the conference focused on translational research and medical applications of physics, it would have been impossible to ignore the discovery by the ATLAS and CMS experiments at the LHC of a Higgs boson – the particle linked to a mechanism that gives mass to many fundamental particles – and the subsequent award of the 2013 Nobel Prize in Physics to two of the theoreticians who proposed the mechanism. Fabiola Gianotti, former spokesperson of the ATLAS experiment at the LHC, opened the conference and captivated the audience with the tale of the many years of Higgs hunting by thousands of researchers across the world. The role of physics and physicists was highlighted also by Ugo Amaldi in his public talk “Physics is beautiful and useful”. The father of the word “hadrontherapy” showed how, following the discovery of X-rays in 1895, fundamental physics, particle therapy and diagnostics became three intertwined yarns: the advances in one field have an impact on the other two. Amaldi concluded his much-appreciated talk by presenting an overview of possible future developments, including “Tulip” – a Turning Linac for Protontherapy – which is a new prototype that aims to supply protons with compact, less-expensive instrumentation. |