The inaugural meeting of the new European ENLIGHT network for cancer therapy research was held at CERN in February. ENLIGHT brings together all of Europe’s leading players in this emerging field.
The European Network for Research in Light-Ion Hadron Therapy (ENLIGHT) has been established to coordinate European efforts in radiation therapy using light-ion beams. Light to physicists, carbon ions are heavy to biologists and were first used to treat patients at the Japanese Heavy-Ion Medical Accelerator Centre (HIMAC) in Chiba, which has been operational for six years. The facility at Germany’s GSI laboratory, which switched on in 1997 (see GSI treats cancer tumours with carbon ions), has also shown that light-ion therapy can be remarkably successful in curing cancer.
Clinicians, oncologists, physicists and engineers from around the world came to the first ENLIGHT meeting to discuss the physics and engineering of particle accelerators and beam systems needed to provide light ions. Following a welcome from CERN’s director-general Luciano Maiani, proceedings began with an address from Jean-Pierre Gérard, past chairman of the European Society for Therapeutic Radiology and Oncology (ESTRO), who said that the meeting could come to be seen as a landmark in the fight against cancer. He drew attention to the “three Cs” that define the advantages of using radiation therapy: cancer care, conservative treatment, and cost. Radiation therapy is used to cure up to 50% of all cancers; it is non-invasive and its side-effects are often short-lived; and it costs just 5% of the total budget for cancer treatment.

Professor Gérard also pointed out that improving technologies are leading to better results. Data from HIMAC and GSI have convinced him that ions are the ultimate weapon for cancer control when no other treatment is possible. If four or five centres were set up, he said, each treating approximately 1000 otherwise incurable patients per year, about 2500 lives could be saved annually. In Professor Gérard’s opinion, working together is the key to success. A concerted effort by physicists and engineers to tackle design issues and by clinicians to deal with patient selection, along with a multidisciplinary approach to imaging, dosimetry and data-handling, has been vital for the success of the two pioneering facilities.
The main aim of radiation therapy is to deliver a maximally effective dose of radiation to a designated tumour site while sparing as much of the surrounding healthy tissue from damage as possible. Conventional radiation therapy using photon beams is characterized by exponential absorption following a maximum, which is reached at a depth of 2-3 cm for beams with a maximum energy of 8 MeV. For selective irradiation of deep-seated tumours, radiotherapists use multiple beams, usually pointing to the geometrical centre of the target area. However, there are still many cases of tumours located near critical organs for which this type of therapy is inappropriate. The dose must be limited to avoid damage to the organ in question, which lowers the chances of successful tumour control.
Hadron therapy
Visionary physicist and founder of Fermilab Robert Wilson first proposed the use of hadrons for cancer treatment in 1946. He observed that unlike photons, protons and light ions deposit their energy at the end of their path and could therefore be used to irradiate tissues close to critical organs. This idea was first put into practice at the Lawrence Berkeley Laboratory (LBL), where 30 patients were treated with protons between 1954 and 1957.
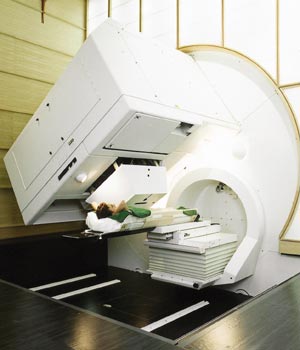
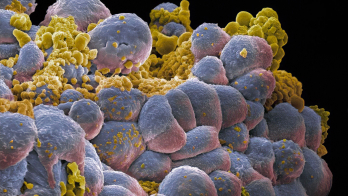
Using beams of hadrons – protons or light ions – radiotherapists can overcome the limitations of photon beams. As well as depositing most of their energy at the end of their range, hadrons penetrate the patient with practically no diffusion and they can easily be formed as narrow-focused and scanned pencil beams of variable penetration depth. This means that they can bring about severe damage to the DNA in cancer cells while sparing both traversed and deeper healthy tissue. This characteristic also enables them to be used to accurately irradiate any part of the tumour. Hadron beams allow highly conformal treatment (in which the beam conforms to the shape of the tumour) of deep-seated tumours to the nearest millimetre, while delivering minimal doses to surrounding tissues.
Since Wilson’s initial proposal, about 30,000 patients have been treated with protons and very good results have been obtained for head and neck tumours. Most of these patients were treated in nuclear research centres not originally designed for cancer therapy. Nevertheless, results have been extremely positive with local control and survival rates higher than those for conventional radiotherapy. At Switzerland’s Paul Scherrer Institute (PSI), an excellent dose delivery system has been developed and integrated in a gantry system that rotates around the patient. The success of therapy projects at nuclear research centres, along with improved accelerator technology and dose delivery systems, has led to a number of dedicated proton therapy facilities being established. These include the Loma Linda University Medical Center in California, US; the Kashiwa and Tsukuba centres in Japan; and the Northeast Proton Therapy Center in Boston, US. At PSI, a second cyclotron is being built exclusively for proton therapy. Known as the PROSCAN project, this facility is due for completion in 2003.
The existing PSI facility is one of Europe’s leading centres for the treatment of melanomas of the eyes and skin, where 60-70 MeV protons are used. Therapy of this nature, in which the tumour is not deep-seated, is well established in Europe, with major facilities in France, Germany and the UK as well as at PSI. Treatment of deep-seated tumours is less well established, and it is this area that the ENLIGHT network will address.